By Michael Ames-Sikora (Editorial Director), Rob Verkerk, Ph.D. (Executive & Scientific Director), and Jonathan Emord, Esq. (General Counsel)
As RFK Jr. and Dr. Makary move to crack down on dangerous ‘herbals,’ like semi-synthetic 7-OH concentrates, sold in gas stations, vape shops, convenience stores, and online, the future of whole leaf kratom, an ancient botanical—and the supplement industry more generally—hangs in the balance.
Listen to the audio version of this article:
THE TOPLINE
- The US has seen an explosion of dubious, addictive, and dangerous unlicensed drugs and adulterated dietary supplements being sold in gas stations, vape shops, convenience stores, and online.
- Last week, the FDA announced the start of a crackdown, initially targeting a derivative of an alkaloid, 7-hydroxymitragynine (7-OH), typically found in minute quantities in the Southeast Asian herb kratom in its whole leaf form.
- Traditional whole leaf kratom preparations are known to be safe and beneficial at low doses, but adulterated products with high concentrations of 7-OH, often semi-synthetically produced, pose serious health risks and are being rightly targeted by the FDA.
- Natural kratom’s future remains uncertain due to regulatory hurdles, despite lack of clear evidence that traditional kratom poses any serious or unreasonable risks.
- Broader implications exist for supplement access, as regulators, particularly at the state level, must avoid using the misuse of isolated compounds to justify blanket bans that threaten other safe, natural botanicals.
Natural kratom, a botanical derived from the leaves of the Mitragyna speciosa tree native to Southeast Asia, has long been used traditionally as a gentle stimulant and mood enhancer. Whether chewed, brewed as tea, or consumed as a water-based extract, kratom has offered centuries of safe use across cultures—particularly in Thailand, Malaysia, and Indonesia. In the US, kratom has gained in popularity for uses such as boosting energy and aiding relaxation. Increasingly, the US has been exposed to ever more concentrated, as well as semi-synthetic, forms of kratom alkaloids, and these have become popular to support drug treatment effects, like alleviating chronic pain or withdrawal from opioid drugs.
Today, kratom’s future in the United States is at a crossroads. How regulators choose to treat products derived or associated with this plant may have sweeping implications for other botanicals that have similar, dose-dependent stimulatory or wellness effects, with important ramifications on the future of dietary supplements and natural health access in general.
A Tale of Two Kratoms
Kratom leaves in their natural form contain a range of alkaloids, most notably mitragynine (MIT). The compound 7-hydroxymitragynine (7-OH) is an oxidation product of MIT and is either non-detectable or present only in trace amounts in kratom leaves or traditional aqueous (water-based) extracts. However, 7-OH can also be produced in the body (via the liver) as a metabolic breakdown product of MIT when the latter is consumed at high doses.
Complicating matters, kratom is a classic example of a ‘hormetic’ herbal: it produces distinctly different effects at low compared to high doses. In low doses, as with traditional preparations, MIT and its associated alkaloids induce a mild, stimulatory, energizing effect and may enhance mental clarity. By contrast, at high doses, MIT and semi-synthetic 7-OH concentrates yield strong, inhibitory, sedative effects characteristic of opioids. The US marketplace for kratom products is now replete with a mind-boggling array of kratom products, some with very high doses of MIT, and others containing isolates of synthetic or semi-synthetic 7-OH that is added as an adulterant. These kinds of products act as opioid drugs because 7-OH is a powerful opioid agonist, up to 13 times more potent, gram-for-gram, than morphine.
In recent years, bad actors selling into and from within the US have been manipulating kratom, producing highly concentrated extracts (isolates), semi-synthetic variants of 7-OH, and the pseudoindoxyl form of MIT that is even more potent than 7-OH. A remarkable array of these kinds of products can now be found across many states in gas stations, vape shops, convenience stores, and online, often being sold alongside the unlicensed drug tianeptine, sometimes referred to as “gas station heroin.” Many, but not all, of the kratom-based products are far removed from the kratom leaf consumed in its traditional, natural form. They are addictive, dangerous, and illegal. Whether they are adulterated dietary supplements or unlicensed drugs, we are strongly of the view that they have no place masquerading as legal dietary supplements on store shelves and online.
That’s why ANH was encouraged to hear of the FDA’s recent enforcement to rein in these harmful products while excluding natural kratom products derived from leaf with no more than trace levels of 7-OH. On July 29, 2025, the FDA recommended that 7-OH be scheduled as a controlled substance by the Drug Enforcement Agency (DEA) due to its opioid-like effects. The states have a patchwork quilt of regulations at odds with the FDA position. Some states ban even whole leaf kratom, like Louisiana, while others regulate ineptly by allowing MIT extracts at high doses that is metabolized in the body exposing users to significant amounts 7-OH, along with allowing concentrated 7-OH to be lawfully sold.
The FDA’s latest position offers clarity, and the states need to avoid conflict with that position and, instead, harmonize their regulations to ban the harmful (semi-synthetic) 7-OH referred by FDA for DEA scheduling, along with extracts that deliver MIT at harmful levels. At the same time, as implicit with the FDA’s approach, states need to preserve citizen access to whole leaf kratom containing alkaloid profiles that are in line with traditional forms of the herbal product.
In the FDA announcement, Dr. Makary stated, “Vape stores are popping up in every neighborhood in America, and many are selling addictive products like concentrated 7-OH. After the last wave of the opioid epidemic, we cannot get caught flat-footed again.”
This latest step by the FDA in effect only targets adulterated products containing concentrates, isolates or semi-synthetic or synthetic forms delivering 7-OH at levels tens or even hundreds of times greater than in traditional preparations. These products are a far cry from natural kratom. We regard this as a landmark decision by the FDA under Dr. Makary’s leadership because it distinguishes specific components (different alkaloids) within a given dietary ingredient (kratom) and so maintains free choice for safe products, while ridding the market of dangerous, adulterated forms of the botanical. We applaud Dr. Makary’s scientific approach to focus enforcement against the harmful but not sweep up into the ban the helpful and safe.
Kratom’s Regulatory Status Remains in Jeopardy
While it’s positive that the FDA has taken this properly nuanced approach, the fact is that access to natural kratom is still under threat. The states variously are not following FDA’s lead on this, banning all kratom, including whole leaf forms. That is a serious mistake that may be pre-empted under the Sixth Amendment’s conflict pre-emption doctrine.
Just as we proposed in our white paper on GRAS, now is the time to introduce a new framework of tiered risk/benefit assessment that takes into account the nuances of different dietary ingredients when consumed in different ways, at different dosages.
In short, while natural kratom may be safe from the FDA’s current crackdown in many states, its future is far from certain in no small measure due to conflicting state enforcement.
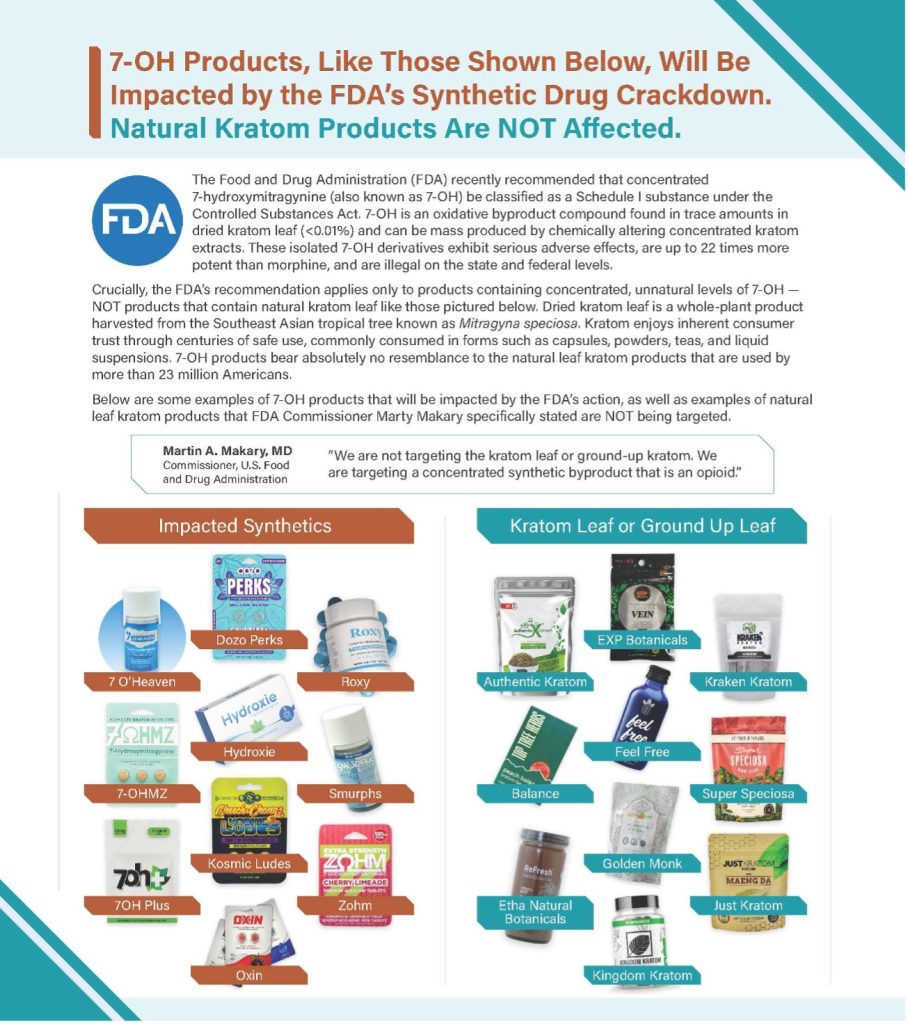
Following is a flier that has been circulating within the kratom industry that attempts to interpret the FDA decision (Disclaimer note: we take no legal responsibility for the contents of the flier as we have not seen validated testing of any of the products shown as examples):
A Precedent with Far-Reaching Consequences
Why does this matter so much? Because kratom is not the only herb with a dose-dependent benefit/risk profile in which low doses give rise to stimulatory effects and high doses inhibitory ones, described scientifically as hormesis. Nutmeg, for instance, is a common culinary spice that becomes psychoactive at high doses. St. John’s Wort affects mood through its influence on neurotransmitters. Valerian root has calming, sedative properties. Kava, yohimbe, Lobelia, chaparral, comfrey, and green tea extracts can all be harmful if consumed at excessive dosages.
If we allow isolated psychoactive effects—or potential for misuse in adulterated forms—to become a basis for blanket bans, we risk undermining the entire supplement category. Could passionflower, Valerian root, lemon balm, resveratrol, curcumin, and a catalogue of herbs from the Ayurvedic and traditional Chinese medicine traditions, such as ginseng, Astragalus, Rehmannia, Cordyceps, Ashwagandha, Tulsi, Triphala, Guduchi and shilajit be next? Well – that’s exactly what’s happening in Europe, and our colleagues at ANH Europe are in the front lines of that battle to save lower doses of these botanical or related ingredients. Given the FDA’s history, it wouldn’t shock us if, ultimately, it ended up protecting the interests of Big Pharma rather than health freedom.
That’s why it’s vital that regulators, lawmakers, and consumers understand the science and draw a clear line between adulterated, lab-generated, dangerous products and natural, traditionally used ingredients and supplements. We believe the legal tools are already available within the adulteration provisions within the Dietary Supplements and Health Education Act (DSHEA) for the FDA to remove dangerous and adulterated products from the market. This task will be made even simpler by the scheduling of 7-OH as a Schedule I controlled substance. Schedule I, which includes heroin, LSD, and ecstasy, is the most restrictive category, reserved for substances that have no currently accepted medical use in treatment, a lack of accepted safety under medical supervision, and a high potential for abuse.
The Science Supports Safe, Traditional Kratom Use
Despite alarmist headlines, toxicity and addiction risks associated with kratom increase primarily with high-dose, long-term use of concentrated extracts or lab synthesized alkaloids—not with moderate consumption of natural kratom.
Indeed, the World Health Organization (WHO) and the European Food Safety Authority (EFSA) have both acknowledged kratom’s potential risks but have not recommended full bans. Lacking authoritative guidance from these or any other institutions, states in the US have been left to deal with the issue themselves. Several states have completely banned kratom while others have passed laws regulating its sale (requiring age restrictions, labeling of MIT and 7-OH levels, product registration, etc.).
But the science, so far, tells us that at low levels of exposure, such as those associated with the traditional use of whole kratom leaf often exhibits beneficial effects with little evidence of any toxicity. At higher exposures, particularly dozens and hundreds of times higher than those made from whole kratom leaf, these responses give way to an array of toxic responses, as well as addiction, especially when accompanied by long-term use. Like the approach outlined in our white paper on Generally Recognized as Safe (GRAS) reform, we need a nuanced approach that preserves access to safe, natural kratom while removing adulterated and dangerous products—not blanket bans that throw the baby out with the bathwater.
When the FDA Gets it Right
ANH applauds the FDA for drawing a firm line against 7-OH-laced products and other kratom formulations that are essentially unapproved drugs masquerading as supplements. These products are illegal, unsafe, and have no place on the market. We commend FDA’s issuance of 7 warning letters to industry members responsible for selling these harmful products and look forward to FDA enforcement to rid the market of them.
At the same time, we urge the FDA, DEA, and policymakers to follow Dr. Makary’s lead by preserving access to natural kratom. The best way to protect consumers and preserve freedom of choice is through self-regulation by responsible industry players coupled with smart, science-based regulation to weed out bad actors—not overreach.
States and retailers need clear guidelines on distinguishing safe, traditional products from dangerous adulterants. Labels should indicate proper dosages and carry precautions for vulnerable populations. And regulators must make it easier for researchers to study natural kratom in context—not just in synthetic isolation.
Protecting Health Freedom Starts With You
The fight over kratom is about more than just one plant. It’s about defending your right to access safe, natural health options in the face of growing regulatory overreach. The FDA’s move to schedule dangerous, highly addictive, lab-synthesized 7-OH is a step in the right direction — but unless we draw a clear line between harmful adulterants and safe, traditionally used botanicals, we risk losing access to many safe herbal products.
For decades, pharmaceutical interests have promoted the idea that only licensed drugs can guarantee safety, effectiveness, and quality—casting doubt on dietary supplements that don’t go through the same pre-market authorization process. But here’s the truth: any unsafe or misbranded dietary supplement is already illegal under US law, and the FDA has the authority to remove it from the market. What we need is enforcement—not new laws that strip away consumer choice.
What You Can Do
- Stay informed: Learn the difference between traditional herbal products and dangerous adulterated ones.
- Support responsible companies: Choose brands that offer lab-tested, traditionally prepared kratom and botanical supplements.
- Contact your state lawmakers: Urge them to follow the FDA’s lead — ban the harmful, preserve the safe.
- Speak up: Tell your community, friends, and networks why this matters. The more voices raised, the harder it becomes to ignore.
This is a critical moment. How kratom is regulated now will set a precedent for how other botanicals — from resveratrol, turmeric, ashwagandha, through kava, yohimbe, green tea extracts and many more — may be treated in the future.
At the Alliance for Natural Health USA, we’re committed to preserving your right to choose natural health pathways. But we can’t do it without you.
Please share this article widely, speak out, and stand up for thoughtful, science-based regulation — not fear-driven bans.
Together, we can protect health freedom for this generation — and the next.




There is not any problem with SAFE traditional non-synthetic Kryptom . The problem is the synthetic is an opiate 13 x more potent than morphine, it hads been put in gummies for children and ecvery other damn thing. It is a precursor to opiate addiction as it is an actyua; OPIATE chemically when engineered by who ever is doing so, and that means it binds to the receptors of cells that normally provide a NATURAL high from the body’s own natural biochemistry meaning that it BLOCKKS those receptors to combat pain, enhance meditiation and spirituality etc ,and has been dsigned to do so to CAUSE addiction.
Will you not share that side of the damn story becasue holistic pain treatments work and it is SYNTHETIC kryptom which is what is being mad made a class 1 and absolutely ought to be.
RFK is making a HUGE mistake banning 7-OH. Now people will run to BigPharma (methadone, suboxone) or a cheaper and more potent illegal alternative: fentanyl (cartels). He literally just shafted the MAHA movement and sold out to AKA…and AKA is hoping people will turn to a “leaf-only” alternative, but the levels required to be effective are toxic. It’s a lose//lose for Americans. Especially those in addiction recovery.