…which is why we need to cultivate our own natural immunity.
THE TOPLINE
- Antibiotic resistant infections are a public health disaster that kill 3,500 people a day globally and are projected to kill 300 million people a year by 2050.
- Big Pharma’s answer is to develop ever more antibiotic drugs to fight these infections, even if bacteria will eventually develop resistance to these new drugs.
- The problem is that mainstream medicine relies too heavily on antibiotics, neglecting the fact that we rely on microbial communities in our gut, mouth, and skin to stay healthy.
- A slew of natural compounds like certain peptides, silver, copper, and botanicals offer alternatives to antibiotics, and it is harder for bacteria to develop resistance to these medicines.
As winter descends upon us, the chill in the air brings more than just frosty winds and snow-laden landscapes; it also heralds the season of heightened vulnerability to infections as we huddle together inside to escape the cold.
If you do get sick, it’s more than likely that your doctor will send you home with a prescription for an antibiotic without any consideration of the reasons why our immune systems come under pressure during the colder months, commonly including lower vitamin D status.
Our health system’s over-reliance on antibiotics to treat routine infections is in part responsible for a looming disaster: antibiotic resistance. Bacteria that are resistant to antibiotic drugs have become a leading cause of death worldwide, killing about 3,500 people a day. Antibiotic-resistant infections are projected to kill an estimated 300 million people by 2050. Unfortunately, yet predictably, rather than turning to natural strategies that optimize our innate ability to fight off pathogens, the conventional medical establishment is racing to develop ever more drugs to fight resistant bacteria, even while acknowledging that it will only be a matter of time before bacteria become resistant to the new drugs.
Consider the recent news of the development by the Swiss drug giant Roche of a new antibiotic, zosurabalpin, for the treatment of carbapenem-resistant Acinetobacter baumannii (CRAB, for short). CRAB is one of those nasty hospital-acquired infections that kills about half of the patients that acquire it. After looking at a set of 45,000 peptide compounds, the researchers honed in on, and tinkered with, one promising candidate that became zosurabalpin. (It’s not all that surprising that the foundation for the new drug is a peptide; several of those that are currently threatened by the FDA have antimicrobial properties).
While the mainstream news has focused on the impressive achievement (it’s been more than 50 years since a distinct class of antibiotic was developed that could treat this kind of bacteria), the scientists themselves urge caution. In their findings, the researchers noted that a gene mutation they observed in the lab that decreased the drug’s effectiveness 256-fold. Roche’s global chief of discovery for infectious diseases told reporters, “Resistance has emerged to every antibiotic ever created, and it is likely that resistance will emerge to zosurabalpin in the future too, if it successfully becomes a clinical antibiotic.”
This is just one example. Drug companies are exploring a variety of avenues to kill bacteria. They are harnessing viruses to do the dirty work, using CRISPR to try to turn bacteria’s defenses against them, while also looking at lab-made peptide nucleic acids (PNAs) to block bacteria from building essential proteins for survival. Of course, artificial intelligence is also being used to identify potential drug candidates for antibiotics.
What this drug-centered approach is missing is that it is the over-marketing and unnecessary overuse of antibiotics that has driven antibiotic resistance. Studies have found that around 30 percent of antibiotic prescriptions are unnecessary. Overuse of antibiotics in industrial agriculture is another problem. Pinning our hopes on the development of ever more drugs to stave off a time when our antibiotics no longer work seems doomed to failure, same as relying on ever more pesticides to grow our food.
The last few decades of research on the human microbiome show we evolved alongside of and rely on microbes to live healthily and to heal. Our immune system is responsible for managing potentially pathogenic bacteria, which comprise only about 5 percent of bacterial species. It’s starting to become common knowledge that our health is intricately connected to the diverse ecosystem of microbes that reside in our gut, mouth, and skin.
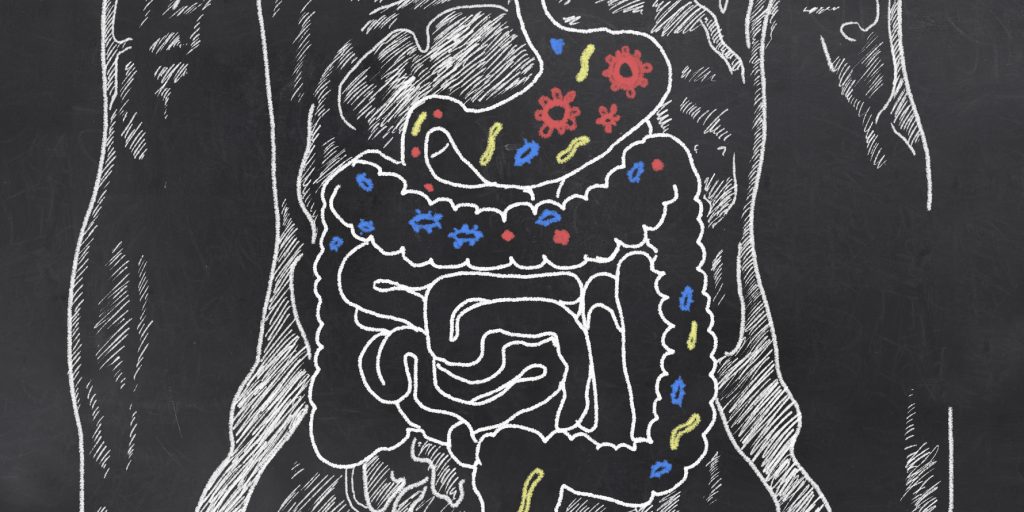
Taking antibiotics for an infection, especially broad-spectrum antibiotics, indiscriminately kills off both pathogenic and “good” bacteria, throwing off this delicate and all-important balance required for good health. And, of course, antibiotics that only target bacteria are often prescribed inappropriately because the source of the infection is viral or fungal — with doctors arguing they’re simply guarding against the risk of secondary bacterial infections while failing to admit they’re contributing to antimicrobial resistance!
Our over-reliance on drugs is a testament to the fact that our natural defense systems have been sabotaged by our modern lifestyles: poor diets, environmental exposures to chemicals and EMFs, lack of sleep and exercise, and stress, all contribute to impaired immunity.
There are also a slew of natural compounds that function effectively as antimicrobials, including peptides, elements like silver and copper, as well as botanicals (garlic, tea tree oil, oregano oil, thyme, and more). Crucially, it is generally harder for bacteria to become resistant to natural medicines like these because natural compounds tent to target multiple biochemical pathways within bacteria, affecting various cellular functions simultaneously. Bacteria would need to mutate in multiple ways to escape these natural antibiotics which is why nature made them that way in the first place! With antibiotic drugs, there is usually just a single mechanism of action that targets one part of the bacteria’s physiology, making it much more likely that rapidly reproducing bacteria will come up with a mutation that gets around the defense creating a so-called ‘superbug’.
Then, of course, there are nutrients that can support overall immunity like those we discussed during the COVID pandemic: zinc, vitamins C and D, quercetin, melatonin, curcuminoids, etc.
Building up our natural ability to ward off harmful pathogens while building healthy microbial communities within us is clearly the baseline to making us as resilient as possible in the face of infectious agents that have the ability to kill us. That requires that we have access to nature, that we don’t live in excessively sterilized environments and that we have good access to the treasure trove of natural medicines. As these can’t be patented and sold for exorbitant sums by drug companies, they just aren’t part of the medical system’s answer. What’s more, two key agencies, the FDA and the FTC, now with the assistance of social media companies, are actively working to block public communications that help the people to learn more about how they can use natural medicines to benefit their health.
Do your friends, family and others in your network a favor: share this article and help them get off the antibiotic treadmill and use natural health as their first line of immune defense.





Thanks Dr. Verkirk and ANH! Well explained and much needed! DR